Article: Dolgin, Elie. 2013. “Antibody drugs set to revive flagging migraine target”. Accessed April 4th, 2013. http://www.nature.com/nrd/journal/v12/n4/full/nrd3991.html

I chose this article to analyze as my published paper #1 since this topic is all too familiar to me, as I myself have suffered with headaches and migraines since the age of 14; 7 years to date. I have researched intensely into this topic hoping for a solution to my own migraines.
This article first begins with the story of Emily S. who began experiencing headaches at age 7. Emily is now 31 years old and her headaches have now turned into severe migraines. Over these 24 years, she has tried a variety of prophylactic cures, none of which proved successful in alleviating her migraines. A prophylactic is a medication or a treatment designed and used to prevent a disease from occurring. These treatments used the anticonvulsant drug, Topiramate. However this drug caused short term memory loss and nausea. This combination of a tricyclic antidepressant and a beta blocker has deemed futile to these attacks.
The initial mechanism.
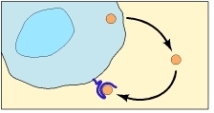
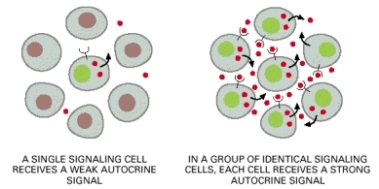
Statistics show that more than 10% of adults in the world experience unbearable migraine headaches. Even though 40% of “migraineurs” are good contenders for therapeutic prophylactic methods, only 1 in 3 of these people receives it. Four monoclonal antibodies (mAbs), currently in Phase I & II, are used to treat these patients, in hope that a problem plagued drug target is what is needed for permanent relief of this problem. These mAbs ultimately hinder the signaling of calcitonin gene-released peptide (CGRP). CGRP is a 37-amino-acid neuropeptide expelled by primary sensory neurons in the trigeminal ganglion during migraine episodes.
Developments.
Small molecule CGRP receptor antagonists have been in development for over a decade. A telcagepant, formulated by Merck & Co. was an investigational drug for the acute treatment and prevention of migraine. This drug gained recognition when it proved to exhibit results superior to placebo when it was used as an abortive therapy in Phase III trials. A placebo effect occurs when a treatment with no known effectiveness, such as a dummy pill, is given to a patient and the patient nevertheless has subsequent improvement in symptoms. However, the company terminated the development of the drug due to escalated liver enzyme transaminase levels in patients that used the drug over an extended period. Nevertheless the trend of using injectable, prophylactic mAbs directed at CGRP or the CGRP receptor is flourishing.
Advancements.
By 2011, companies such as Amgen and Arteaus Therapeudics began testing new routes for the drug to target; the mAb directed at the CGRP peptide itself. Most recently, in January of 2013, Labrys licensed their drug to the renowned Pfizer Company. They postulated the dosage of once a month. “An antibody with a long half-life” said Alder’s pharmacists, a competing firm. Since the antibodies were not chemically similar to CGRP but instead blocked it, there would be no trace of liver problems.
Concerns.
Fears stemmed from the concern that the CGRP-directed mAbs would not cross the blood-brain barrier (BBB). This simply meant that the drug might not have a significant effect on the neurons in the brain. This apprehension was quickly dismissed on the view that both the peripheral and central systems could be stimulated instead of either or. Another issue was the presence of side effects. Due to CGRP’s ability to heal wounds easily, neuroscientists pondered upon the consequences of depleting the peptide and its long term effects. In the end it was decided that the drug would only prosper after the clinical benefits and injuries were evaluated, with the advantages outweighing the disadvantages. Despite the drug’s high cost of production, it earned more 10,000 times more than its initial cost in profits. In conclusion, the drug proved worthwhile for companies such as Artaeus amidst of generic market of mAbs.
Additional references: